Understanding Medicare Appeals: Level 1 Redetermination
Introduction
Navigating Medicare claims can be a complex process, especially when a claim is denied and needs to be appealed. The first step in the Medicare appeals process is known as Level 1: Redetermination. This stage is critical as it sets the foundation for any subsequent appeals. This blog aims to provide a comprehensive guide to understanding the Level 1 redetermination process, including how to file an appeal, what to expect, and tips for success.
Overview of Medicare Appeals Process
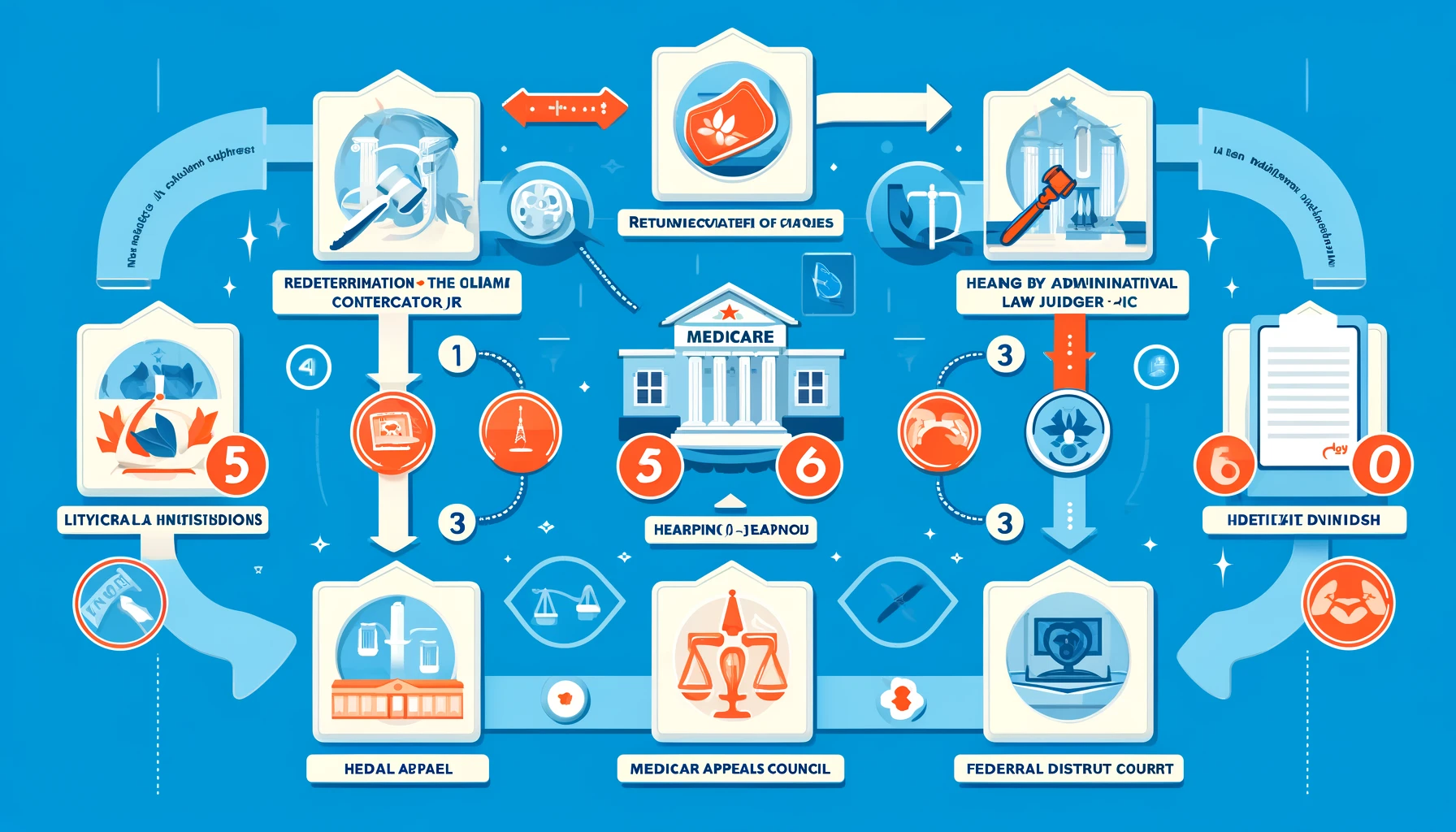
The Medicare appeals process is structured to ensure that beneficiaries have multiple opportunities to contest a denied claim. The process consists of five levels:
- Level 1: Redetermination by the Medicare Administrative Contractor (MAC)
- Level 2: Reconsideration by a Qualified Independent Contractor (QIC)
- Level 3: Hearing by an Administrative Law Judge (ALJ)
- Level 4: Review by the Medicare Appeals Council
- Level 5: Judicial Review by a Federal District Court
This blog will focus on Level 1: Redetermination.
What is Level 1: Redetermination?
Redetermination is the first level of appeal in the Medicare claims process. It involves a re-examination of a denied claim by the same company that initially handled it. This company is known as the Medicare Administrative Contractor (MAC). The goal of redetermination is to provide a quick and efficient review of the initial decision.
Reasons for Filing a Redetermination
There are several common reasons why a Medicare claim might be denied, leading to the need for a redetermination:
- Lack of medical necessity: The MAC may determine that the service or item provided was not medically necessary based on the information available.
- Incorrect coding: Errors in the coding of the service or item can result in denial.
- Insufficient documentation: If the required documentation is not provided or is incomplete, the claim may be denied.
- Non-covered services: The service or item may be excluded from Medicare coverage.
How to File a Redetermination Request
Filing a redetermination request involves several steps:
- Review the Medicare Summary Notice (MSN): This notice will explain why the claim was denied and provide instructions on how to file an appeal.
- Complete the Redetermination Request Form (CMS-20027): This form can be obtained from the Medicare website or requested from the MAC.
- Include Supporting Documentation: Gather any additional medical records, doctor’s letters, or other documents that support your case.
- Submit the Request: Send the completed form and supporting documentation to the address provided by the MAC within 120 days of receiving the MSN.
Tips for a Successful Redetermination
To increase the chances of a successful redetermination, consider the following tips:
- Be Thorough: Ensure that all sections of the Redetermination Request Form are completed accurately and that all necessary documentation is included.
- Provide Detailed Justifications: Clearly explain why you believe the claim should be paid, referencing specific medical records or other evidence.
- Meet Deadlines: Submit your request within the 120-day window to avoid automatic denial.
- Seek Professional Help: Consider consulting with a healthcare advocate or an attorney who specializes in Medicare claims if you need assistance.
What to Expect After Filing
Once the redetermination request is filed, the MAC will review the information and make a decision. The MAC has 60 days from the date of receipt to notify you of their decision. There are three possible outcomes:
- Full Reversal: The MAC agrees with your appeal and overturns the initial denial.
- Partial Reversal: The MAC partially agrees with your appeal and approves part of the claim.
- Denial: The MAC upholds the original decision to deny the claim.
If the redetermination is denied or only partially approved, you have the right to escalate the appeal to Level 2: Reconsideration by a Qualified Independent Contractor.
Common Challenges and How to Overcome Them
Filing for redetermination can be challenging due to various factors. Here are some common challenges and strategies to overcome them:
- Complex Medical Records: Ensure all medical records are clear and well-organized. Highlight relevant sections to make it easier for the reviewer to understand your case.
- Incomplete Documentation: Double-check that all required documents are included with your request. Missing documents are a common reason for denial.
- Miscommunication: Maintain open lines of communication with your healthcare provider to ensure you have all necessary information and documentation.
- Deadlines: Mark important dates on your calendar and set reminders to avoid missing the 120-day filing deadline.
Case Study: Successful Redetermination Appeal
To illustrate the redetermination process, let’s look at a hypothetical case study.
Background: John, a Medicare beneficiary, had a claim denied for a knee replacement surgery, which was deemed not medically necessary by the MAC.
Steps Taken:
- Reviewed MSN: John carefully reviewed the denial reasons listed in his MSN.
- Gathered Documentation: John obtained a letter from his orthopedic surgeon detailing the medical necessity of the surgery, along with preoperative and postoperative medical records.
- Completed CMS-20027: John filled out the Redetermination Request Form with the help of a healthcare advocate.
- Submitted the Request: He mailed the form and supporting documents to the MAC within the required timeframe.
Outcome: After 45 days, John received a notification from the MAC that his redetermination request was successful. The denial was overturned, and Medicare covered the cost of his knee replacement surgery.
Resources for Assistance
If you need help with filing a redetermination request, several resources are available:
- Medicare Website: Provides forms, instructions, and contact information.
- State Health Insurance Assistance Program (SHIP): Offers free, personalized counseling and assistance.
- Legal Aid Organizations: Provide help for low-income individuals needing assistance with Medicare appeals.
- Healthcare Advocates: Professionals who specialize in navigating healthcare claims and appeals.
Conclusion
Understanding and navigating the Medicare redetermination process can be daunting, but with the right knowledge and resources, it is manageable. By following the steps outlined in this guide, you can increase your chances of a successful appeal at the first level. Remember to be thorough, provide detailed justifications, and seek assistance if needed. With persistence and attention to detail, you can effectively handle a Medicare claim denial and secure the coverage you are entitled to.
Additional Information
For more detailed information and access to forms, visit the official Medicare website or contact the Medicare Administrative Contractor for your region. Stay informed about your rights and options to ensure you receive the best possible care and coverage under Medicare.