Understanding Appeals for Medicare Health Plans
Navigating the intricacies of Medicare can be challenging, especially when it comes to appealing decisions related to coverage or payments. If you disagree with a decision made by Medicare or your Medicare health plan, you have the right to appeal. This blog will guide you through the appeals process, explain your rights, and provide tips for a successful appeal.
Table of Contents
- Introduction to Medicare Appeals
- What is a Medicare Appeal?
- Why Might You Need to File an Appeal?
- Types of Medicare Health Plans
- Original Medicare
- Medicare Advantage Plans (Part C)
- Medicare Prescription Drug Plans (Part D)
- Medigap (Medicare Supplement Insurance)
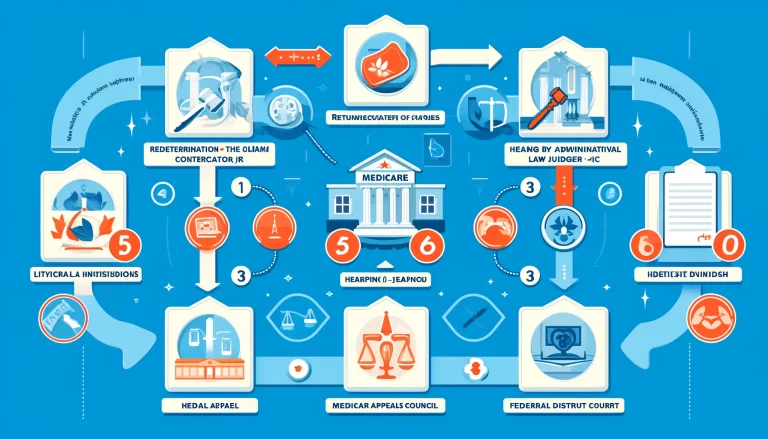
- The Five Levels of Appeals
- Level 1: Redetermination by the Medicare Administrative Contractor (MAC)
- Level 2: Reconsideration by a Qualified Independent Contractor (QIC)
- Level 3: Hearing by an Administrative Law Judge (ALJ)
- Level 4: Review by the Medicare Appeals Council
- Level 5: Judicial Review by a Federal District Court
- How to File an Appeal
- Step-by-Step Guide to Filing an Appeal
- Important Deadlines and Timelines
- Common Reasons for Appeals
- Denial of Coverage for Medical Services
- Disputes Over Payment Amounts
- Prescription Drug Coverage Issues
- Hospital Discharge Disputes
- Tips for a Successful Appeal
- Gathering and Organizing Documentation
- Writing a Clear and Concise Appeal Letter
- Seeking Assistance from SHIP and Other Resources
- Frequently Asked Questions (FAQs)
- Can Someone File an Appeal for Me?
- What if My Appeal is Denied?
- How Long Does the Appeals Process Take?
- Additional Resources
- Contact Information for Medicare Assistance
- Useful Links and References
1. Introduction to Medicare Appeals
What is a Medicare Appeal?
An appeal is a formal request asking Medicare or your Medicare health plan to review and reconsider a decision regarding your healthcare coverage or payment. If you believe that Medicare or your plan has made an incorrect decision, you can challenge it through the appeals process.
Why Might You Need to File an Appeal?
There are several reasons why you might need to file an appeal, including:
- Denial of coverage for a medical service, treatment, or prescription drug.
- Disagreement with the amount Medicare or your plan will pay for a service.
- Concerns about the quality of care received.
- Issues with hospital discharge decisions or length of stay.
2. Types of Medicare Health Plans
Original Medicare
Original Medicare includes Part A (Hospital Insurance) and Part B (Medical Insurance). It is managed by the federal government and provides coverage for many healthcare services and supplies.
Medicare Advantage Plans (Part C)
Medicare Advantage Plans are offered by private companies approved by Medicare. These plans provide all Part A and Part B benefits and often include additional coverage like vision, dental, and prescription drugs.
Medicare Prescription Drug Plans (Part D)
These plans add prescription drug coverage to Original Medicare, some Medicare Cost Plans, some Medicare Private-Fee-for-Service Plans, and Medicare Medical Savings Account Plans.
Medigap (Medicare Supplement Insurance)
Medigap policies are sold by private companies and help pay for some of the costs that Original Medicare doesn’t cover, such as copayments, coinsurance, and deductibles.
3. The Five Levels of Appeals
The Medicare appeals process consists of five levels. Each level provides an opportunity for a different entity to review the decision.
Level 1: Redetermination by the Medicare Administrative Contractor (MAC)
A redetermination is an independent review of an initial claim decision by the MAC. If you disagree with the original decision, you can request a redetermination.
Level 2: Reconsideration by a Qualified Independent Contractor (QIC)
If you disagree with the MAC’s redetermination, you can request a reconsideration. A QIC, an independent entity, will review your case.
Level 3: Hearing by an Administrative Law Judge (ALJ)
If you disagree with the QIC’s decision, you can request a hearing before an ALJ. The amount in controversy must meet a minimum threshold for an ALJ hearing.
Level 4: Review by the Medicare Appeals Council
If you disagree with the ALJ’s decision, you can request a review by the Medicare Appeals Council. This is an independent review within the Department of Health and Human Services.
Level 5: Judicial Review by a Federal District Court
If you disagree with the Council’s decision, and the amount in controversy meets a minimum threshold, you can request a judicial review in a federal district court.
4. How to File an Appeal
Step-by-Step Guide to Filing an Appeal
- Review the denial notice: Carefully read the denial notice to understand why your claim was denied.
- Gather documentation: Collect all relevant documents, including medical records, doctor’s letters, and any correspondence related to your claim.
- Complete the necessary forms: Fill out the appropriate appeal forms. For Original Medicare, use Form CMS-20027 for redeterminations.
- Submit your appeal: Send your completed forms and supporting documents to the address provided in the denial notice. Make sure to keep copies for your records.
- Follow up: Monitor the status of your appeal and be prepared to provide additional information if requested.
Important Deadlines and Timelines
- Redetermination: Request within 120 days from the date of the initial decision.
- Reconsideration: Request within 180 days from the date of the redetermination decision.
- ALJ Hearing: Request within 60 days from the date of the reconsideration decision.
- Medicare Appeals Council: Request within 60 days from the date of the ALJ decision.
- Judicial Review: Request within 60 days from the date of the Council’s decision.
5. Common Reasons for Appeals
Denial of Coverage for Medical Services
You might need to appeal if Medicare or your plan denies coverage for a medical service or treatment you believe is necessary.
Disputes Over Payment Amounts
Appeals can be filed if you disagree with the amount Medicare or your plan is willing to pay for a service.
Prescription Drug Coverage Issues
If your Medicare drug plan denies coverage for a medication, you can appeal the decision.
Hospital Discharge Disputes
If you feel you are being discharged from the hospital too soon, you can appeal the discharge decision.
6. Tips for a Successful Appeal
Gathering and Organizing Documentation
- Collect all relevant medical records, bills, and correspondence.
- Keep a detailed record of phone calls and conversations related to your appeal.
Writing a Clear and Concise Appeal Letter
- Clearly state why you are appealing.
- Include supporting documentation and reference relevant medical records or doctor’s notes.
- Be specific about the decision you disagree with and what you are requesting.
Seeking Assistance from SHIP and Other Resources
- Contact your State Health Insurance Assistance Program (SHIP) for free counseling and assistance.
- Consider hiring a Medicare advocate or attorney if your case is complex.
7. Frequently Asked Questions (FAQs)
Can Someone File an Appeal for Me?
Yes, you can appoint a representative to file an appeal on your behalf by completing an Appointment of Representative form (Form CMS-1696).
What if My Appeal is Denied?
If your appeal is denied at any level, you can proceed to the next level of appeal. Each level provides another opportunity for review.
How Long Does the Appeals Process Take?
The time frame for each level of appeal varies. Redeterminations typically take about 60 days, while ALJ hearings can take several months.
8. Additional Resources
Contact Information for Medicare Assistance
- Medicare Customer Service: 1-800-MEDICARE (1-800-633-4227)
- State Health Insurance Assistance Program (SHIP): Varies by state; check online for local contact information.
Useful Links and References
By understanding the appeals process and knowing your rights, you can take the necessary steps to ensure that you receive the coverage and care you need. If you face any challenges or have questions, don’t hesitate to seek assistance from Medicare resources or legal professionals specializing in healthcare appeals.