The Inpatient-Only List Explained: A Game Changer in Healthcare
We’re diving into a nuanced yet crucial topic in the healthcare sector: the Inpatient-Only List, as regulated by Medicare CMS. This list, encompassing around 1,800 codes for procedures that must be conducted on an inpatient basis, has seen significant changes over the years, impacting how healthcare facilities operate and compete.
Understanding the Inpatient-Only List
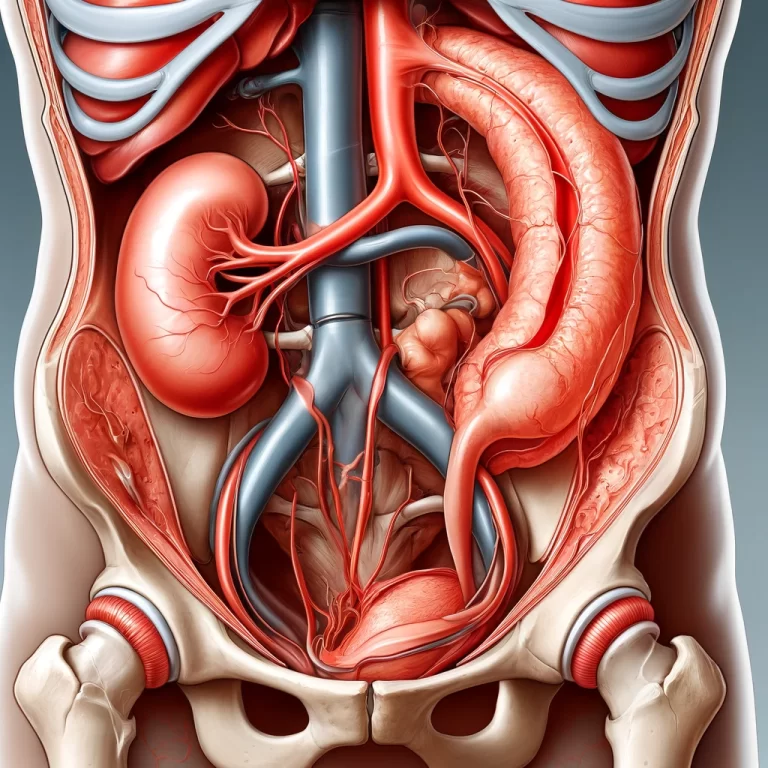
The Inpatient-Only List specifies procedures, like complex coronary artery bypass grafts, that require hospitalization for at least two midnights, adhering to what’s known as the “two midnight rule.” These are procedures you can’t have done at an Ambulatory Surgery Center (ASC) because they necessitate an inpatient stay.
However, a shift began in 2021 when CMS started to remove procedures from this list. By 2024, further codes were eliminated, allowing for more procedures to transition from inpatient to outpatient settings, notably in ASCs. This evolution is significant because it opens the door for non-hospital-owned ASCs to perform these procedures, intensifying competition with hospital systems.
The Financial Implications and Strategic Responses
The financial implications and strategic responses of hospital systems to the evolving landscape of inpatient and outpatient care are pivotal in understanding the current and future state of healthcare delivery. As the Medicare CMS changes the Inpatient-Only List, removing certain procedures that can now be performed on an outpatient basis, hospital systems face a significant shift in their operational and financial models.
Financial Implications
- Revenue Reallocation: Traditionally, inpatient procedures have been a major revenue stream for hospitals. These procedures tend to be more costly and, therefore, more profitable. With the shift towards outpatient care, hospitals risk losing a substantial portion of this revenue.
- Cost Structure Adjustment: Transitioning to more outpatient procedures requires hospitals to adapt their cost structures. Outpatient care generally requires less overhead compared to inpatient care, prompting hospitals to rethink resource allocation, staffing, and facility usage.
- Investment in ASCs: Recognizing the trend towards outpatient care, major hospital systems like Hospital Corporation of America (HCA) and Tenet Healthcare are investing in Ambulatory Surgery Centers (ASCs). This not only helps them retain a foothold in the profitable procedure market but also allows them to cater to the growing demand for outpatient services.
Strategic Responses
- Expansion of ASC Networks: By expanding their network of ASCs, hospital systems can capture the outpatient market, ensuring that they remain competitive and relevant. This expansion is not merely about increasing numbers but also involves enhancing the quality of care, incorporating advanced technologies, and improving patient experiences in these settings.
- Diversification of Services: Hospitals are diversifying their service offerings to include more outpatient procedures, which requires them to adapt their facilities and invest in new technologies and training for their staff.
- Partnerships and Acquisitions: Some hospital systems are forming strategic partnerships or acquiring existing ASCs to fast-track their expansion into the outpatient space. These moves are strategic, aiming to leverage the expertise and operational efficiencies of established ASCs.
- Competitive Pricing Strategies: As more procedures move to outpatient settings, there’s increased price transparency and competition. Hospitals are thus motivated to devise competitive pricing strategies for outpatient services, ensuring they remain attractive to patients and insurers.
- Focusing on Quality and Patient Satisfaction: With the shift towards outpatient care, hospitals are placing greater emphasis on quality of care and patient satisfaction. The outpatient setting offers a more patient-centered, convenient, and often less stressful environment, which can lead to better patient outcomes and higher satisfaction rates.
The shift from inpatient to outpatient care is reshaping the financial and strategic landscape for hospital systems. Adapting to these changes requires a multifaceted approach, involving investment in ASCs, service diversification, strategic partnerships, competitive pricing, and a strong focus on patient-centered care. As hospital systems navigate this transition, their ability to adapt and innovate will be key to their continued success and relevance in the healthcare industry.
The Impact on Healthcare Finance and Patient Care
The transition of procedures from inpatient to outpatient settings, particularly in the context of Ambulatory Surgery Centers (ASCs), is significantly impacting healthcare finance and patient care. This shift is especially relevant for self-funded employer health plans, which bear the direct cost of healthcare services used by their employees. Let’s delve deeper into the nuances of these impacts.
Impact on Healthcare Finance
- Cost Reduction Opportunities: Moving procedures to outpatient settings can lead to substantial cost savings. Outpatient care generally requires fewer resources than inpatient care, including shorter stays and less intensive use of hospital facilities and staff. For self-funded employers, this translates to lower medical expenses for the same procedures, enhancing the overall sustainability of their health plans.
- Variability in Costs: While outpatient procedures are generally less expensive, the cost can vary significantly depending on the ASC’s ownership and contractual agreements. Procedures performed at ASCs under hospital contracts often mirror the hospital’s pricing structures, which can be substantially higher than those at independent ASCs. This variability underscores the need for employers to understand and strategically choose their healthcare partners.
- Direct Contracting: To harness the cost benefits of outpatient care, self-funded employers are increasingly considering direct contracting with independent ASCs. Such contracts allow employers to negotiate rates, ensuring more predictable and lower costs for procedures without compromising on quality. Direct contracting also offers employers the leverage to include quality and performance metrics in their agreements, aligning financial and health outcomes.
Impact on Patient Care
- Quality of Care: Independent ASCs often provide high-quality care with a focus on specific types of procedures, which can result in better patient outcomes. For instance, a physician-owned ASC specializing in knee replacements will likely have a team that’s highly experienced in that specific procedure, benefiting patients through specialized care.
- Patient Experience: Outpatient care is typically more convenient and patient-friendly. It involves shorter wait times, quicker discharge processes, and the comfort of recovering at home, all of which contribute to a better overall patient experience.
- Access to Care: Independent ASCs can increase access to care by offering more locations and often shorter waiting times for procedures. For employees covered by self-funded health plans, this means they can receive necessary treatments faster, reducing downtime and improving health outcomes.
- Transparency and Choice: Direct contracting with ASCs can offer more transparency in healthcare costs and outcomes, empowering employers and patients with information to make informed decisions. This level of transparency and the ability to choose from a range of providers can enhance satisfaction and engagement in one’s own healthcare journey.
A Specific Example
Consider the case of a physician-owned ASC in Texas providing knee replacements at a fraction of the cost compared to hospital-affiliated ASCs. This scenario illustrates not just the potential for significant cost savings but also the benefits of specialized care. Patients receiving treatment in such facilities benefit from the focused expertise of healthcare providers who perform these procedures regularly, potentially leading to better outcomes and faster recovery times.
The shift towards outpatient procedures in ASCs presents a nuanced landscape for healthcare finance and patient care. For self-funded employers, it’s a call to strategically navigate this landscape, balancing cost, quality, and access to care, while for patients, it represents a shift towards more convenient, efficient, and potentially higher-quality care options.